So the Supreme Court said 'sex' means 'biological sex'. That means no more mixed-sex hospital wards, right? Right?
And our hospitals will be places where we are safely cared for, with privacy and dignity at all times. Yes? Well...
I didn’t think I’d write about this topic. In fact I’d intended to publish the conclusion of my ten step career pivot series this weekend. But the news over the last few days seems to be perpetuating a series of misunderstandings about hospital admissions, single sex wards, ‘private’ rooms and what might be about to change. So it feels important to speak up just now.
This essay is long, because there are many details about how admissions are organised in the NHS that are not necessarily widely understood, but to be able to form an opinion on something as controversial as this, it’s vital to be clear about what - if any - change it is that we’re asking for. So it’s one to read with a cuppa and a spare twenty or so minutes. Or to listen to on your commute, perhaps.
In the wake of last week’s Supreme Court ruling, clarifying the specific meaning in law of the terms ‘woman’ and ‘sex’ as used in the 2010 Equality Act, there has understandably been much discussion and debate around single sex spaces, with one particular space causing concern and sensational headlines being hospital wards.
With current NHS guidance recommending that trans people be admitted to wards according to their gender identification, the judges’ ruling on ‘woman’ referring to ‘biological woman’ and ‘sex’ referring to ‘biological sex’ has led to calls for immediate changes to policy.
On Thursday, the Health Secretary was interviewed on LBC radio1. Though I cannot say that I agree with all that Wes Streeting has had to say in the past on the NHS, I was surprised to be quite impressed with the way he handled this particular conversation, on the whole giving a rather balanced and compassionate view on a remarkably difficult topic.
Speaking To Ben Kentish on LBC radio, Streeting said:
“We want to make sure that we’ve got single sex provision and wards in the NHS, and that’s based on biology, and to make sure that trans people have access to safe and dignified and respectful care.
The NHS is updating its guidance and what we would like to see is appropriate kinds of rooms and private spaces for trans people to be cared for in NHS hospitals.”
- Wes Streeting, speaking on LBC radio 24 April 2025
Several news outlets interpreted these comments as a suggestion that transgender patients would be treated in private rooms23 with even the LBC interviewer pressing Streeting on the prospect, suggesting that some might consider it ‘unfair’ if trans patients were to be ‘prioritised’ and cared for in single rooms a sentiment that appears to be echoed in headlines seemingly intended to achieve little more than to stoke outrage.
After 18 years working as a surgeon in the NHS, I wanted to add a little real life experience to explain what the deal is with single sex spaces in the NHS, why there has been a reported increase in ‘breaches’ of the single sex accommodation policy and to put all of this into some context.
Because the truth is that every single decision about where each individual patient is cared for is a considered one. Often balancing multiple, competing needs. I have heard more than once in jest, that managing beds in hospitals is akin to rearranging deck chairs on the Titanic. On days when capacity is tightest (and there are few days in present times when this is not the case), it can feel very much as though the ship is going down whatever we do.
What do the guidelines say?
To specifically examine the rules relating to single sex spaces in hospital, let’s start with the evolution of the current guidelines, contained in a document titled ‘Delivering same sex accommodation’, published by NHS England in September 20194.
Guidance recommending admitted patients in NHS hospitals be cared for in single sex accommodation was first introduced in 2009. Even in the early noughties though (I joined medical school in 2001), the vast majority of hospital wards - or at least rooms (bays) within wards, were single sex, though this was not specifically monitored at the time.
The cited reason for introduction of the guidance was the ‘safety, privacy and dignity of patients’, a statement repeated in Streeting’s interview, and given top of billing in the foreword of the current iteration of the document.
Every patient has the right to receive high quality care that is safe and effective and respects their privacy and dignity.
- NHS England, Delivering same sex accommodation
Streeting emphasised that [prevention of] violence against women and girls is the main reason for the existence of the same sex accommodation regulations.
One of the reasons that we have to tread carefully in this area, and sensitively, is for two things. Firstly, in terms of violence against women and girls, the reasons why we have sex-based rules for the NHS, quite apart from anything to do with gender identity, is because even in the NHS, we still see far too much male violence against women and girls including sexual violence and harassment in the NHS settings where women should be safe. And secondly… I heard a pretty harrowing report of a trans man, so this is someone who was born a girl, lived his life as a man, wanted, understandably given that, to be on a male ward for his treatment. In one ward [he] was physically attacked by someone else on the ward because they recognised that he wasn’t born a man. And on another occasion in another ward, someone tried to sexually assault him, because his genitalia hadn’t changed… and that’s why this whole question about safety and dignity really matters.
- Wes Streeting, speaking on LBC radio 24 April 2025
Reporting of ‘breaches’ of the guidance - episodes of mixing of male and female inpatients - became mandatory in April 2011, with fines of £250 levied to hospitals per person accommodated in a mixed bay. These rules were adopted into the NHS Constitution (2012), NHS Standard Contract (2013) and Clinical Quality Commission reviews (2014) over the coming years. The guidance was updated in 2019 to provide more specific information on when mixing might be considered justified on clinical grounds, as well as clarification of specific considerations for ‘trans people and gender variant children’, drafted with the support of the Government’s Equalities Office.
Trans people should be accommodated according to their presentation: the way they dress, and the name and pronouns they currently use.
Let’s park that particular clarification for now. It may be the statement that is causing the most controversy at this moment, but there is more to understand before we dig into that sandpit.
First - let’s understand what is ‘allowed’ and what is categorised as a ‘breach’?
Detailed guidance can be found here.
In summary -
Sleeping, toileting and bathing areas for ADMITTED adult patients are single sex.
What does NOT count as a breach though?
Time in the Emergency Department
Time on a decision-making (whether to admit or not) ward such as a medical or surgical assessment unit
Critical care wards - because clinical need makes mixing in these areas justifiable in the guidance
Importantly, for these latter two exceptions, once a decision is made to admit a patient (from the mixed-sex assessment area) or step down to a normal inpatient ward (from a mixed-sex area of critical care), if the transfer takes longer than four hours, this is then counted as a breach of the single sex accommodation guidance.
For children and young people, the guidance suggests that patients (parents if the child is very young) should be able to choose whether they are cared for in a single- or mixed-sex space. In practice, every children’s ward I have worked on is mixed-sex throughout, though a particular individual request would be accommodated where practicable.
So to summarise and paraphrase the practical interpretation of the rules:
Hospital adult inpatient ward sleeping, toileting and bathing facilities should be single-sex spaces.
Critical care is not single-sex (unless step-down to ward takes more than four hours from being declared ‘ready’)
Assessment areas are not single-sex (unless transfer to ward takes more than four hours from decision to admit)
Children’s wards are not single sex
The Emergency Department is not single sex
Second question then, has the requirement to accommodate men and women separately made NHS hospitals safer, in terms of sexual assault or harassment?
Well, it’s difficult to say, as the occurrence of sexual crimes in hospitals is not routinely collected data.
Hold on one moment. Let’s just read that again.
The occurrence of sexual crimes in hospitals is not routinely collected data.
Hospitals are required to return to a central, mandatory register, reports of mixed-sex ‘breaches’. But no such reports are required for rape.
Let’s imagine a male patient who has spent two weeks in a mixed-sex bay in intensive care and who is now recovering. He is seen on the ward round one morning, and the consultant decides that he is well enough to step down to a standard ward. Four hours later, he is still in the same bed on intensive care, waiting for a bed on a male ward to become available. Now the hospital must report this case to the central NHS register as a mixed-sex accommodation ‘breach’.
But if a patient is sexually assaulted or harassed, that will be dealt with according to local policies and procedures, with or without involving the police, but NO central register of such incidents exists.
Are we missing the point on what’s actually important, here?
So what information is available?
There have been separate studies which provide some information:
A National Patient Safety Agency report5 in 2006 documented 19 suspected rapes and more than 100 sexual safety incidents on NHS mental health wards over a two year period. Of these, in 8 of the rape cases the alleged perpetrator was another patient; in 11 it was a member of staff. 20 of the cases related to reports of consensual sex.
An investigation6 by Sky News and the Independent who collated data via freedom of information requests sent to mental health trusts in England found nearly 20,000 sexual safety incidents between 2019 and 2023, with numbers rising each year - there were nearly 4000 such incidents between January and August 2023.
In acute trusts, a BMJ study7 documented 35,000 reports of sexual assault and harassment between 2017 and 2022, with 62% of these incidents being against staff and 48% against patients. 20% of the incidents involved patients as both victim and perpetrator, with 9% involving staff members allegedly assaulting or harassing patients.
It is difficult to interpret this information with any specificity, as the data collection methods differ, the denominator is not reported, it is possible that different types of incidents are included in each investigation, the data sets are incomplete and none are directly comparable. What this does tell us is that the NHS is not as safe, in terms of sexual safety, as anyone might hope; that distressingly, many incidents involve staff as alleged perpetrator, that it appears that sexual safety is not significantly improved since the guidance was introduced, and that data on this really very important type of event is not routinely collected.
So if it’s no safer, is that because the single sex accommodation guidance is not being followed?
Well, firstly, there is clear evidence that the number of breaches of the guidance is increasing.
As discussed, data on breaches is returned monthly by every NHS trust and reported publicly by NHS England8.
The green line on the chart below illustrates the reported instances of mixed sex accommodation breaches across the NHS in England.
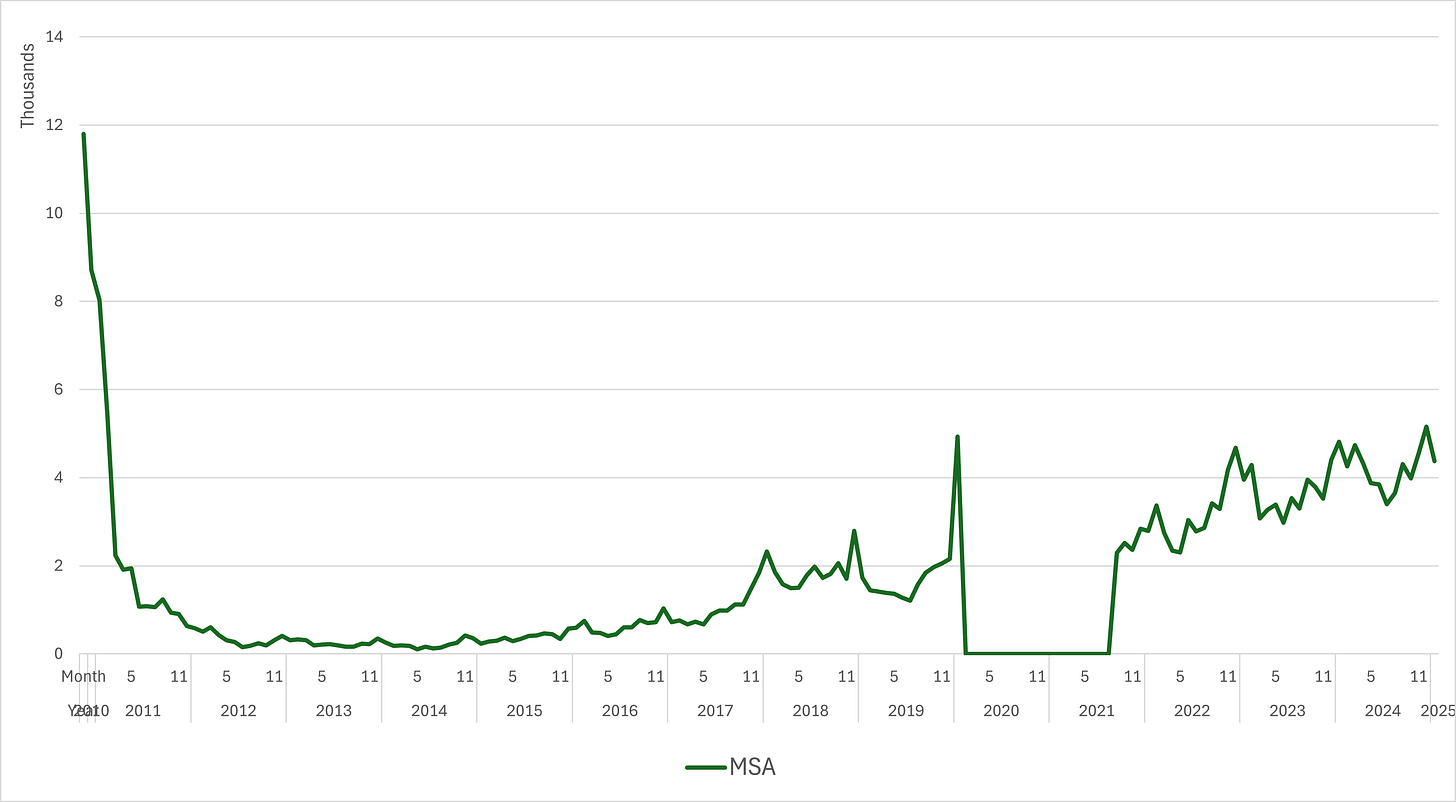
It is instantly apparent that documented breaches reduced once mandatory reporting - and fines - were introduced in April 2011, and the numbers remained suppressed for around 3-4 years before creeping up again. The annual upward spikes tend to correspond with the winter months, when bed pressures are known to be highest across the NHS. Notably, fines for breaches were not reintroduced even once monitoring recommenced after the pause on both at the height of the pandemic. What is also clear from a single glance at this chart is that breaches are increasing - and that this drift upwards began well before the word ‘lockdown’ landed on anyone’s lips.
So what’s going on here then?
What I can tell you, whether this is reassuring or not, is that hospitals are not just carelessly admitting patients in to mixed sex bays and wards. In fact, such a thing is almost unheard of.
What I strongly suspect is the case - a suspicion supported by personal experience as well as some specific evidence I’ll share with you - is that the vast majority of these breaches are a result of delays in transferring patients who are waiting for a bed, because the beds are not available. So remember, these are not patients waiting in ‘A&E’. They don’t ‘count’ for this type of breach. These are the patients waiting in mixed sex assessment ward areas for more than four hours after a decision to admit. (And those first four hours of waiting, and the 4/8/12/however many hours waiting for that decision to be made, don’t count). Or, they’re the patients waiting more than four hours for a step down bed from critical care - who may have spent days/weeks/longer in that particular mixed-sex space.
The majority of instances of mixing of sexes is quite simply down to delays waiting for a bed in an appropriate ward or bay.
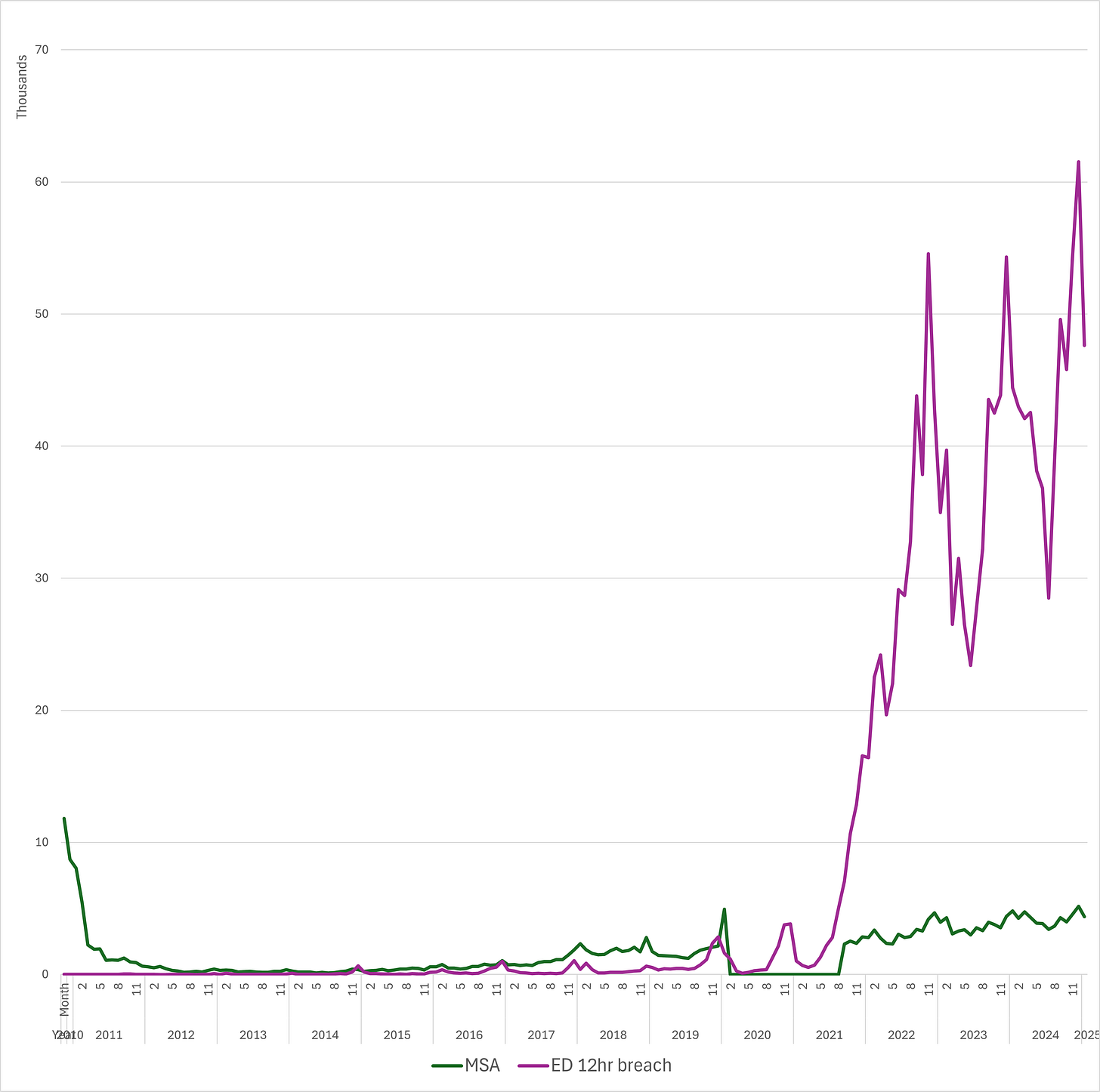
Let’s take a look at this chart, where as well as the mixed-sex breaches we saw above, I’ve added on a purple line to represent what’s happening in the Emergency Department.
So the purple line shows how many patients are spending more than 12 hours in the Emergency Department. In my first decade of practice as a doctor, it was unheard of for patients to spend 12 hours in ED. There was intense pressure to admit or discharge patients even before the four-hour mark, and this requirement had its own specific target with a fine attached for ‘breaches’.
Indeed, I recall in my first years of practice, a management consultancy firm were called in to review the ED where I worked to try to reduce the four hour target breaches as the fines were costing the hospital so much money. The consultancy team spent several weeks wandering around with NHS managers (identifiable by their clipboards), and produced a report at a cost of £several million, which recommended (in short) “more doctors, more nurses, and more space”. Well. Who’d have thought?
So, because a shiny expensive report suggested it, the hospital did in fact invest in implementing the recommendations. The orthopaedic team were evicted from fracture clinic to open up a large space adjacent to the ED (I suppose they were found space elsewhere, but I try to stay away from fracture clinic as much as humanly possible, so I couldn’t tell you where they put them). And lots of extra shifts were put out to locum at inviting rates - around £50-60 per hour for a second year doctor, in 2006. Many doctors more senior than that struggle to be paid anywhere near those figures for additional shifts almost 20 years on.
And the results? 4 hour breaches were reduced to near-zero. And the money that the hospital spent on the consultancy report PLUS the locum and overtime costs was covered more than fivefold by the savings on breach fines. Most importantly, the patients got a better deal. Anyway, that was a little aside, but I thought it helpful to illustrate some context and to emphasise that the 12 hour breaches rising off the scale as they are is really a Very Big Problem.
They are a problem for a lot of reasons, but mostly, because there is no space to care for patients, which means corridor care, and because there is no space to care for patients, which means queues of ambulances outside unable to offload their patients and get back out to attend the next call, and because there is no space to care for patients, which means clinical staff spend more time looking for patients, and negotiating hospital trolleys like tetris pieces to find a cupboard (not an exaggeration) private enough to examine someone, rather than actually, you know, seeing the patients, and THERE IS NO SPACE TO CARE FOR PATIENTS.
There is nothing safe, or private, or dignified about any of this.
Given this knowledge, it is not in the least surprising then that there are more mixed-sex accommodation breaches. In fact I think I’m actually surprised that there aren’t more.
I promised some specific evidence to back up what I suspect is causing these breaches.
Here are responses directly from hospital trusts when asked to explain surges in mixed-sex breaches:
This one reported in The Standard, from East Sussex NHS Foundation Trust in 2012
A statement from the trust said there were a few days in October when there was a "sudden surge in severely ill patients" needing admission to the hospital.
The statement read: "This led to one of our day units being used to admit inpatients requiring an operation. The trust is committed to minimising cancelled operations and, for this short period of time, exceptional measures were introduced to ensure patients requiring an operation could be admitted.
"Whilst from a quality perspective, patients were cared for well, some patients had to change behind closed curtains into theatre gowns in order to go to theatre. This breached Department of Health guidelines of same-sex accommodation."
and this one from the Royal Berkshire Hospital, reported in the Reading Chronicle in February 2020
“We have well established guidelines to make sure all our patients, parents and carers are treated with dignity and respect and their privacy is preserved whilst they are using services at the RBH.
"The mixed sex breaches recorded here have been in our Acute Medical Unit and are caused by high attendance levels in our Emergency Department when we have to move patients quickly to prevent overcrowding.
"There have not been any mixed sex ward breaches anywhere else in the hospital.
Ok. Now let’s imagine you’re a hospital manager for a second.
ED have 20 patients who have been waiting overnight for a ward bed. 10 of these need a surgical bed. To keep things simple, 5 of them are men, 5 are women.
The surgical ward has 10 available beds. 7 are in male bays, 3 in female bays. But there is a post-op lady waiting to step down from critical care who also needs one of those beds. And two ladies on the surgical admissions ward who have been waiting 3.5 hours to come to the ward.
What do we do? Leave the ladies on the admissions ward and critical care where they are a little longer, and admit the 5 men and 3 of the women from ED to the ward beds, probably, because at least being in an admissions ward or critical care is safer than being in ED. But what if critical care need the bed for a new admission? And we’re still leaving two women in ED, for how long, 24 hours? More? At least we have two male beds available on the ward. Well, for now. They won’t last long. The deckchairs on the Titanic analogy makes more and more sense the more you think about these daily, impossible situations. Every one of these patients is a vulnerable, unwell, human. It could be you, or I, or our mother or brother or child. And no solution is ideal.
In our imagined scenario, what if one of the 5 men is actually a trans man. They ask to be admitted to a male ward. The current guidance supports that request. But then there’s the Supreme Court ruling… so now what? There are male beds available. There are no female beds available. Well, didn’t Wes say they should go in a private room?
So what about single rooms then? How many are there? Who is using them?
Just considering overnight beds for now, there are 133,846 beds available in total in the NHS as of the most recent figures from Oct-Dec 20249. Just 2,200, or 1.6% of these are single patient rooms10.
These are unequally distributed across hospitals, with newer buildings usually hosting a greater proportion of single rooms. Two hospitals - Royal Tunbridge Wells, and the new Royal Liverpool Hospital, are understood to have solely single rooms11. But single rooms have their downsides - they require more staff to safely observe them, and many patients complain of isolation. So even if it were affordable to reconfigure or rebuild every hospital, there are arguments to be weighed about the pros and cons12.
In an older hospital, on a traditional ward of around 28 beds, a more typical arrangement would see between two and six of those beds being located in single rooms.
These single (or ‘side’) rooms are utilised for a number of specific reasons:
To isolate patients who are suffering from or carriers of contagious illnesses
To isolate patients who are especially vulnerable because of immunodeficiency, so would be at risk in an open bay (such as those undergoing stem cell transplant for example)
To safeguard children admitted to adult wards (it is common for young people aged 16-17 to be admitted to adult services, though they are legally children and require specific safeguarding measures and accommodations such as the facility to allow a parent to stay with them)
To provide private and dignified end of life care
To provide appropriate accommodations for patients with specific learning and sensory needs, or mental health needs, who may be especially disoriented or distressed in an open bay
AND
To accommodate patients whose gender identity does not match their biological sex: this is not new. Every trans patient I have ever met in a hospital environment has been cared for in a side room. Of course, it may not be the case that every trans patient has been in a side room in every hospital on every admission, but I suspect that the majority, where possible, are. The reason for this, despite the Supreme Court ruling being so recent, is that, as I wrote at the beginning of this essay:
Because the truth is that every single decision about where each individual patient is cared for is a considered one. Often balancing multiple, competing needs.
One more story to illustrate this point, before I finish.
I worked on a small (adult) ward with 18 beds, just two were side rooms. One side room was being used by a 17 year old male, recovering from very major surgery, whose mother was staying with him. The other was occupied by an elderly lady in her last hours to days of life. The intensive care unit needed to step down a sixteen year old girl to the ward, who as well as needing a side room because of her age, also had Covid, so needed a side room for isolation. There was no good solution. Every possible option was debated. In the end, I negotiated with critical care, the ward sister, the bed manager and the paediatric bed manager to explore potential temporising measures, and we agreed that critical care would keep her there overnight, and she would come to the planned ward if the side room was vacant by then, otherwise would go to the paediatric ward who had a space, but where care would be more challenging because her treating team were based on the adult service. Because she stayed in critical care (a mixed area) for more than four hours after she was fit for step down, that would have been recorded as a mixed sex breach. These discussions took at least twelve phone calls over several hours.
NHS staff care deeply. The core of every decision is that we try to do best by as many patients as is humanly possible. And throughout, patients are kept updated and involved in decisions about their care, as they should be.
So what’s likely to change in practice, as a result of the Supreme Court ruling?
In practice, honestly, very little I suspect. Except probably some even more challenging decisions for our NHS ward sisters, hospital bed managers, and at times, doctors, who may have to step in as I did in the case above to decide the clinically ‘least bad’ option.
Because the problem is simple, though the fix is sadly not.
There are not enough beds. Or at least, not enough flow to be able to discharge patients from hospital beds.
There are not enough side rooms.
Every day is a juggling act.
Everyone is doing their best.
And to make sure we don’t lose sight of what is actually important, we should remember that just because something is measured (or measurable), that doesn’t make it the only thing that matters. What actually matters, when considering single sex spaces in hospitals? Privacy, dignity and safety. Not a political soundbite. Not a fear-stoking newspaper headline. Not a politician’s personal legacy.
So on this, the last word goes to a young woman who was, in her words ‘groomed and sexually abused by a male member of staff at a child and adolescent psychiatric unit’. I consider her words equally applicable to acute care trusts as to the mental health trusts she refers to.
Nima Cas Hunt writes13
…the suggested implementation of single-sex wards appears to be a politically-fuelled “sticking-plaster” solution to what is, in reality, a complex, deep-rooted and systemic issue plaguing the UK’s mental healthcare system…
…Segregating male and female patients overlooks the institutional factors that lead to an environment where patients aren’t safe; if these factors go unchallenged, then abuse of patients, in all its forms, continues to happen. Single-sex wards can’t fix systematic malpractice.
Privacy. Dignity. Safety.
At the moment, these are not guaranteed anywhere in the NHS. And nothing that the Supreme Court judges said has changed that. If only it were that simple.
Let’s remember what we’re asking for.
This is a really difficult topic to think about, and to write about. I have been fortunate to find readers who offer thoughtful commentary on everything I’ve written, and I hope that this will be no different.
If you’d like to read more essays like this, this is the button you’ll need.
I’ll be back soon with the final part of my career pivot essay series. I hope you’ll forgive my slight detour. In some ways, writing this piece has been helpful in planning exactly what I need to say in that final essay. There are certain topics where I feel a responsibility to use the hard earned experience I have to speak up, and so that will need to be a part of the next steps in the work I’m called to do. It’s a journey, that much is for sure. I hope you’ll join me.
NPSA 2006 [ARCHIVED CONTENT] With safety in mind






WOW Louise.... just WOW. I'm in absolute awe of you. What a meticulous piece of writing. You know what I think of you, you're all real life superheroes to me. I can only imagine the multi-faceted judgement calls that have to be made about what HUMAN gets what space. What you deal with is just unimaginable. I bow down to you, I really do.
It was a really interesting read. Having spent a lot of time at our local hospital over the last few years (4x90+year old parents/in-laws) I’ve witnessed the bed allocation issues and seen the results of the lack of investment in adult social care that leaves frail old people waiting for days for discharge until a suitable place can be arranged for them. However, the overwhelming impression is of the care and kindness of the staff who are obviously doing their very best for the patients.